Your Guide to Ejection Fraction and the Subtle Signs to Know
Ejection fraction is a simple-sounding percentage that can reveal a lot about how well your heart pumps blood. Understanding what it means, how it is measured, and which subtle symptoms can signal strain helps you have clearer conversations with your care team and track meaningful changes over time.

Your Guide to Ejection Fraction and the Subtle Signs to Know
Heart function is often discussed in numbers, and few are referenced as often as ejection fraction. While it is only one part of the story, it can help explain why certain symptoms show up and how clinicians in cardiology think about risk and treatment options. Learning the basics can also reduce confusion when test results change slightly from one visit to the next.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is ejection fraction and why it matters?
Ejection fraction (EF) describes the percentage of blood the left ventricle pumps out with each heartbeat. It does not measure how much blood is in the body overall; it focuses on the heart’s pumping efficiency per beat. A lower fraction can suggest weakened pumping, while a normal fraction does not automatically rule out heart-related symptoms. EF is most often discussed for the left ventricle because it supplies the body, but right-sided pumping can matter too.
EF is useful because it helps group patterns of heart dysfunction and can guide which therapies are considered. Still, it should be interpreted alongside symptoms, blood pressure trends, lab results, and other imaging findings. A single number rarely captures the full picture, especially when conditions like valve disease, rhythm problems, or long-standing hypertension are involved.
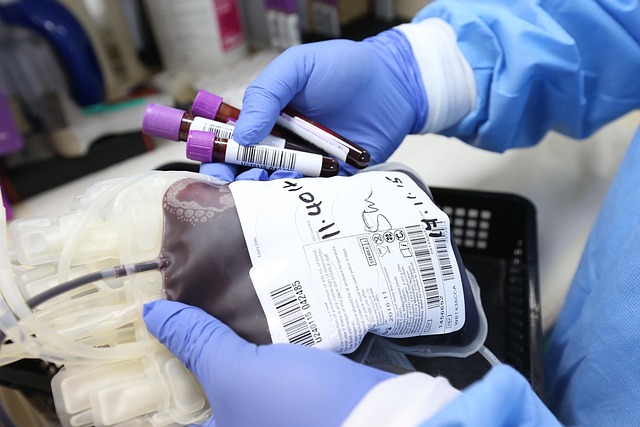
How an echocardiogram measures the ventricle
An echocardiogram is an ultrasound test that creates moving images of the heart. It helps clinicians estimate EF by measuring how the ventricle changes size between relaxation and contraction. The test can also evaluate valve function, wall motion, chamber size, and signs that fluid pressures may be elevated. Because it is noninvasive, it is commonly used for diagnosis and follow-up.
EF values can vary slightly depending on image quality, the method used, and even the heart rate at the time of the exam. That is why trends over time and the written interpretation can be as important as the single percentage. In some situations, additional imaging (such as cardiac MRI) may be used to clarify structure or scarring, but the echocardiogram remains the typical starting point.
Fatigue, swelling, and dyspnea: subtle signs
Some of the most easily overlooked symptoms are fatigue, swelling, and dyspnea (shortness of breath). Fatigue may feel like reduced stamina, needing more rest after routine errands, or difficulty keeping up with normal activity. Swelling often shows up in the ankles or lower legs and may be noticed when socks leave deeper marks than usual. Dyspnea can be subtle at first, appearing only with stairs, brisk walking, or lying flat.
These symptoms are not specific to one diagnosis, and they can overlap with lung conditions, anemia, deconditioning, or medication effects. However, when they occur together, worsen gradually, or change quickly over days, they are meaningful to report. In clinical visits, describing when symptoms occur, what triggers them, and how quickly they resolve can be more helpful than assigning a severity score.
Arrhythmia and blood pressure signals to watch
Arrhythmia can change how effectively the heart fills and pumps, sometimes causing palpitations, lightheadedness, chest discomfort, or sudden exercise intolerance. An irregular rhythm can also worsen shortness of breath or fatigue, even if EF is only mildly reduced or appears normal. Because symptoms can come and go, clinicians may recommend rhythm monitoring tools such as a Holter monitor or event monitor to capture episodes.
Blood pressure is another major factor that influences heart workload. Persistently elevated blood pressure can strain the ventricle over time, while blood pressure that drops too low may contribute to dizziness or weakness, especially after medication changes. Tracking home readings with a validated cuff and bringing a log to appointments can help clinicians distinguish day-to-day variability from a sustained trend that needs attention.
Sodium, diuretics, and cholesterol basics
Dietary sodium can affect fluid balance, and some people are more sensitive to sodium than others. Higher sodium intake can contribute to fluid retention, which may worsen swelling and dyspnea. Clinicians often discuss practical approaches such as reading nutrition labels, limiting highly processed foods, and being consistent day to day rather than making abrupt changes that are hard to maintain.
Diuretics are medications that help the body remove excess fluid through urination. They are commonly used to relieve congestion symptoms, but dosing may need adjustment based on weight changes, kidney function, and electrolyte levels. Separately, cholesterol management is part of lowering overall cardiovascular risk, especially when coronary artery disease contributes to cardiology concerns. Decisions about cholesterol-lowering therapy depend on an individual’s risk profile, not EF alone.
Exercise, sleep, and monitoring in daily life
Appropriate exercise can support cardiovascular health, but it should match a person’s current status and clinician guidance. Many people do well with gradual, consistent activity such as walking, light cycling, or structured cardiac rehabilitation when recommended. The goal is often improved functional capacity and symptom stability, not pushing through breathlessness or dizziness. If exercise consistently triggers dyspnea, chest discomfort, or near-fainting, that is a signal to reassess.
Sleep quality matters because poor sleep can worsen fatigue and may be linked with conditions like sleep apnea that influence blood pressure and heart strain. Home monitoring can also be useful: tracking daily weights, swelling, and symptom changes can provide early clues about fluid shifts. A simple routine—same scale, same time of day, consistent notes—can make patterns easier to recognize and discuss during visits.
Ejection fraction is a valuable measurement, but it is most informative when paired with symptoms, test details, and overall cardiovascular risk factors. Understanding how an echocardiogram estimates EF, recognizing subtle changes like fatigue or swelling, and paying attention to rhythm and blood pressure patterns can make health conversations more precise. With steady monitoring and individualized clinical guidance, EF becomes one part of a clearer, more complete picture of heart function.